The only known cure for sickle cell disease
Hello Everyone and Welcome to my blog! I will be posting on various health topics including sickle cell disease which is very close to my heart. I hope to spread awareness about sickle cell anemia and to be an advocate for those who are still waiting for better treatment and curative options. Today I will be talking about my son Landon, who was diagnosed with sickle cell three years ago, 2 weeks after his birth (2019). I will also share our journey and how my husband and I made the decision to pursue a bone marrow transplant for Landon to cure sickle cell.
Landon was only 17 months old when he had his bone marrow transplant which was August 6th, 2020. Landon was given a second chance, a rebirth in a sense, to live a normal life where he is free from pain and progressive organ damage. So it is my responsiblity to create memories for him and to have answers for my children one day when they are old enough to understand. I want them to see that I didn’t just move on with my life after Landon was cured. I want my children to see that life is not only about your victories. It’s also about using the gifts that God gave you to help others in whatever you way you can, and making the decision to live on purpose.
Before I get into how my husband and made the decision to pursue a bone marrow transplant for Landon, I want to walk you through some historical milestones for sickle cell disease and the alarming statistics.
What is Sickle cell disease?
Sickle cell disease was first discovered in the 1900s and it is the most common inherited blood disorder affecting about 100,000 Americans, mostly of African descent and 20 million people worldwide. Sickle cell disease is a single gene defect in which the shape of red blood cells become deformed. Instead of having round and flexible red blood cells people with sickle cell have inflexible, deformed red blood cells.
In 1984, a child with leukemia and sickle cell disease had a bone marrow transplant. She was the first sickle cell patient cured from a bone marrow transplant. That was over 30 years ago.
So why are so many people still suffering with this chronic, life-threatening medical condition?
The truth is for many years there was little interest and little to no funding for sickle cell disease and research to focus on treatment and curative options. This is largely due to the existing racial disparity and the fact that people who are affected by SCD are mostly of African American descent. In the 1970s, one of the great achievements of the civil rights movement was to create the Sickle Cell Disease Association of America, which led to the Sickle Cell Anemia Act of 1972. Since then, there has been more public awareness of the genetic disorder with some improvement in funding towards better treatment and curative options, but it is still not enough.
So what do I mean when I say it’s still not enough?
Let’s look at the statistics. There are 100k people in the US with sickle cell disease and 20 million worldwide. Bone marrow transplant might be an option for at least one third out of the 20 million people with sickle cell disease. That is a significant number.
So you might be asking yourself how many bone marrow transplants have been done to cure sickle cell disease?
This number is fluid because there is more awareness in recent years but from the information sources I have seen only about 2,000 people with sickle cell anemia have undergone bone marrow transplants. So imagine how many lives could be changed if we had enough worldwide support and more funding.
Do you know what else is shocking?
- It is shocking that with all the medical advancement we have made for so many medical conditions, we have yet to have enough interest and the funding to come up with better medications to slow organ damage in sickle cell patients. There is also the issue of having more accessible curative options.
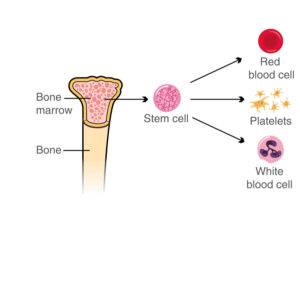
- Bone marrow transplant is an option that comes with great risks but in this case the benefits outweigh the risks particularly in younger patients. Only 20 to 30 percent of children who need a transplant have a matching sibling who can donate but we are not getting that the majority of that 20 to 30% to transplant.
- Medical evidence shows that younger patients (less than 16 years old), and patients transplanted more recently (after 2006) had better outcomes with less complications. The most recent studies show that the cure rate for children with sickle cell disease undergoing a BMT with a matched sibling donor is about 95%. Another way to look at it is on average when 10 children with SCD underwent a matched sibling BMT, 9 out of 10 children were cured.
- In 2018, we saw more progress when the National Heart, Lung, and Blood Institute (NHLBI) launched the Cure Sickle Cell Initiative to accelerate the development of gene therapy, to provide more accessible curative options for people with sickle cell disease. There is a lot of optimism around gene therapy and so far the results in preclinical and clinical trials are promising.
How did my husband and I make the decision to pursue bone marrow transplant for Landon?
The more recent studies showed that the cure rate for children with SCD with a matched sibling donor is about 95%. The benefits of the transplant far outweighed the risks from our perspective. This might not be how others feel but we certainly felt that we were willing to take a chance at Landon being cured as opposed to the alternative of the unpredictable course of SCD and possibly losing him at a young age.
What is a matched sibling donor?
A matched sibling donor describes either a brother or sister who shares the same mother and father that have an identical immune system blood type. There is a blood type for your immune system called human leukocyte antigens (or HLA). These antigens are proteins on most cells in our body and our immune system uses these proteins to see which cells belong in our body and which cells do not belong. When they see cells that don’t belong they signal the immune system to attack those cells and clear them from the body. This is what happens if donor and recipient do not have matching proteins which is not what we want. So when someone is being evaluated for a bone marrow transplant they test HLA proteins for the donor and the recipient. In our case, avery and landon had HLA typing done to see if she was a match for Landon. Landon was 5 months old and Avery was 3 years old at that time. Avery turned out to be a perfect match for Landon so there was less concern that Landon would reject Avery’s cells. It can still happen but less likely if the donor and recipient are a full match.
What does bone marrow mean?
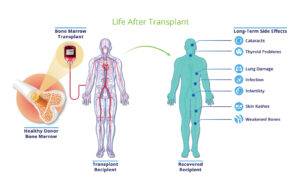
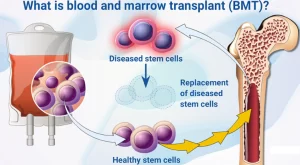
Bone marrow is soft, spongy tissue in the center of our bones. This is where most of our body’s cells are made and stored. Stem cells are the body’s “raw materials” that are found in our bone marrow. All other cells including our nerve cells and blood cells come from stem cells. So that is why bone marrow transplant and stem cell transplant are used interchangeably. The stem cells are what is needed in a bone marrow transplantL(BMT) to cure certain types of cancers and other non-cancer conditions such as sickle cell disease. If the bone marrow doesn’t function properly because of cancer or another disease, a bone marrow transplant may be an option for some people. In the case of sickle cell disease, BMT has been proven to be very successful in patients younger than 16 years of age.
What was the preparation process leading up to the BMT like?
The preparation for Landon’s bone marrow transplant was between 1 to 3 months prior to the date of his bone marrow transplant. Within that period of time, the doctors ordered different tests to check how his different organs were working, to make sure his body was able to handle the bone marrow transplant.
The next phase was for Landon’s first round of chemotherapy 3 weeks before his transplant. So he was admitted mid-july for his first round of chemotherapy. The week before his transplant he was given chemotherapy which was necessary to clean out the bone marrow. For example, the chemotherapy that Landon received has been shown to be effective in preventing rejection of new donor cells. So this chemotherapy along with the other two chemotherapy medications helped Landon’s body to not reject Avery’s cells (his sister).
Landon also needed to go to the Operating room L(OR) for the placement of a big intravenous (IV) line in a large vein near his heart (this is called a central line). This big IV is necessary for giving multiple medications including chemotherapy effectively, and other medications that cannot be given through a smaller iv line. This big IV line is also necessary because if Landon got really sick and needed a lot of medications, and life saving measures this line provides access to deliver medications quickly and effectively.
We also consented to participating a study for testicular preservation options. We consented to the removal of a small piece of Landon’s testicular tissue to be stored (frozen) for fertility preservation. This procedure was done at the same time the central line was placed.

So after Landon’s first round of chemotherapy, he was discharged from the hospital and returned 12 days later for his second admission. During his second admission he received more chemotherapy and 8 days later he had the bone marrow transplant, so remained in the hospital for about 6 weeks.
So you might be wondering what the bone marrow transplant day was like?
It was an insane time because we were in the middle of the pandemic so this of course added a layer of stress to the entire process. In Landon’s case, they used Avery’s umbilical cord blood that was collected at the time of her birth and they did a bone marrow harvest to get more cells from her bone marrow because the umbilical cord cells were not enough for the transplant. Avery was 10 days away from her 4th birthday when she donated her bone marrow cells to Landon. She was given medications to put her to sleep and she was taken to the operating room where they collected her stem cells from her hip bone. They collected the stem cells with a needle that is placed into the marrow. This process is called bone marrow harvest or bone marrow procurement. The stem cells were sent of the lab to go through a filtering process. Once the filtering process was complete, the cells were then ready to be given to Landon. My husband stayed with Landon on the bone marrow transplant unit because Landon was only 17 months old so a parent had to be with him at all times. I waited in a different section of the hospital until Avery returned from the OR. When Avery returned from the OR and woke up from the anesthesia she did not complain about any pain and was pretty much herself. It was quite remarkable. I have a video of her a few hours after the bone marrow harvest which is posted on my Youtube channel.
Landon received Avery’s umbilical cord blood cells and the fresh stem cells harvested from Avery the same day and 2 years later, he is cured and off all medications.
That was our process leading up to Landon’s bone marrow transplant. I have posted an anniversary video on my Youtube channel which can be found at link below. Please sign up with the Be The Match registry if you are interested in donating.
Leave a comment